Progression of Parkinson’s Disease
While there are common symptoms associated with Parkinson’s disease (PD), each individual’s journey with PD is unique. It is difficult to predict the exact symptoms you may experience, when those symptoms may occur, and how severe the symptoms may be. In this blog post we will discuss typical patterns of progression associated with PD.
Prior to Diagnosis
It is common for individuals with Parkinson’s to experience non-motor symptoms years before they seek medical attention for motor symptoms.
Individuals may have noticed:
Loss of smell or taste
Constipation
Fatigue and sleep disorders (active dreams, insomnia, etc.)
Mood disorders
Dysautonomia (orthostatic hypotension)
Often time of Diagnosis
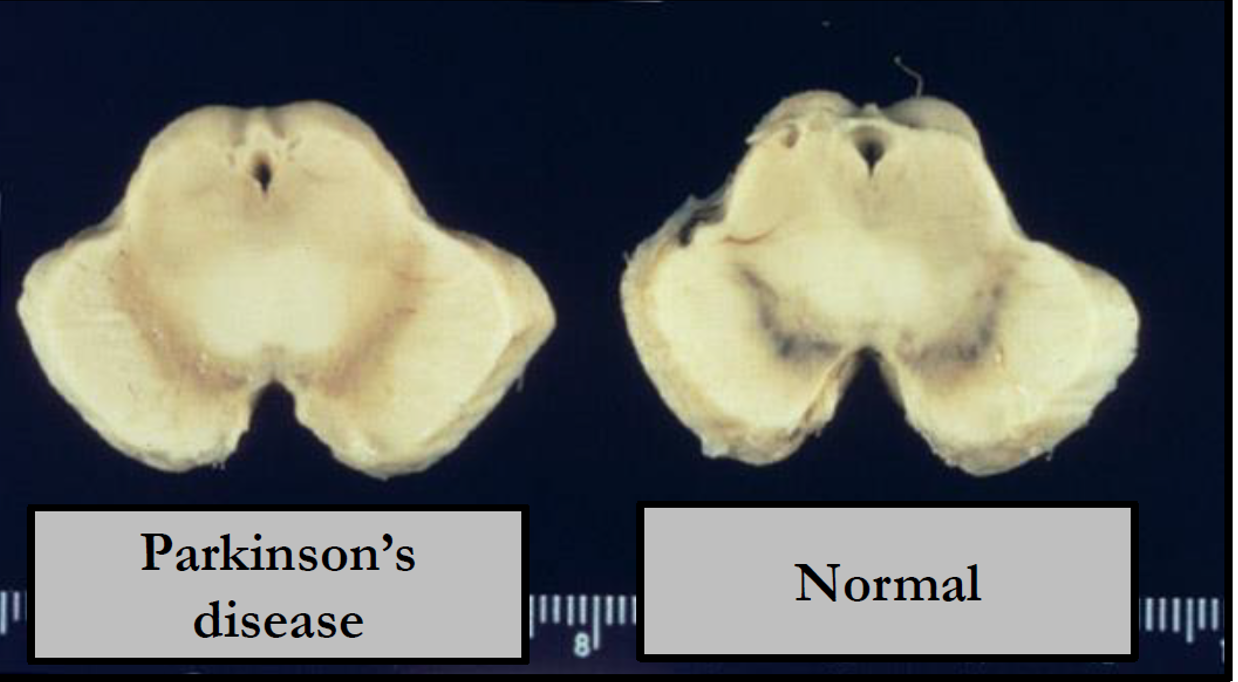
Loss of dopaminergic neurons in the substantia nigra pars compacta leads to Parkinsonian symptoms. 60-80% loss of dopaminergic neurons occurs before onset of the physical signs.
Cardinal Motor Signs:
Tremor
Rigidity
Akinesia/bradykinesia
Postural instability
In the image below, the X (horizontal) axis shows the percent of dopaminergic neurons and the Y (vertical) axis shows time in years of age. Those with Parkinson’s begin losing dopaminergic neurons before the motor symptoms first appear (at the dopamine level threshold).
Staging and Progression of Parkinson’s Disease
Hoehn and Yahr
This is the most widely accepted scale for describing the progression of symptoms in Parkinson’s disease. The initial scale was developed in 1967 with 5 stages and revised/expanded in 2004 to include 7 stages.
Stage 1: Mild symptoms that don’t tend to interfere with activities of daily living. Tremors and changes in posture, walking, and facial expression can occur.
Stage 2: Tremor, rigidity, and motor symptoms affect both sides of the body. Impairments in posture and walking may be more noticeable.
Stage 3: Balance impairments and slowness of movement are noted. Physical independence is maintained.
Stage 4: Needs assistance with activities of daily living and unable to live independently.
Stage 5: Stiffness throughout the body may make functional mobility impossible. Supervision and assistance required.
It is important to note that oftentimes with the appropriate medical management and an appropriate exercise routine, the later stages on this Hoehn and Yahr Scale can be prevented.
Unified Parkinson’s Disease Rating Scale
This is currently the gold standard for quantifying symptoms and progression of Parkinson’s disease. It was initially developed by an international panel of neurologists in the 1990’s and revised by the Movement Disorder Society in 2008 to incorporate the more clinically pertinent items (MDS – UPDRS).
The MDS-UPDRS has 4 parts:
Non-motor experiences of daily living
Motor experiences of daily living
Motor examination
Motor complications
Items are rated from 0 (normal) to 4 (most severe impairment).
Pictured above is the Substantia Nigra in individuals with Parkinson’s Disease vs a healthy norm. The decrease in neurons is shown.
Management of Parkinson’s Disease
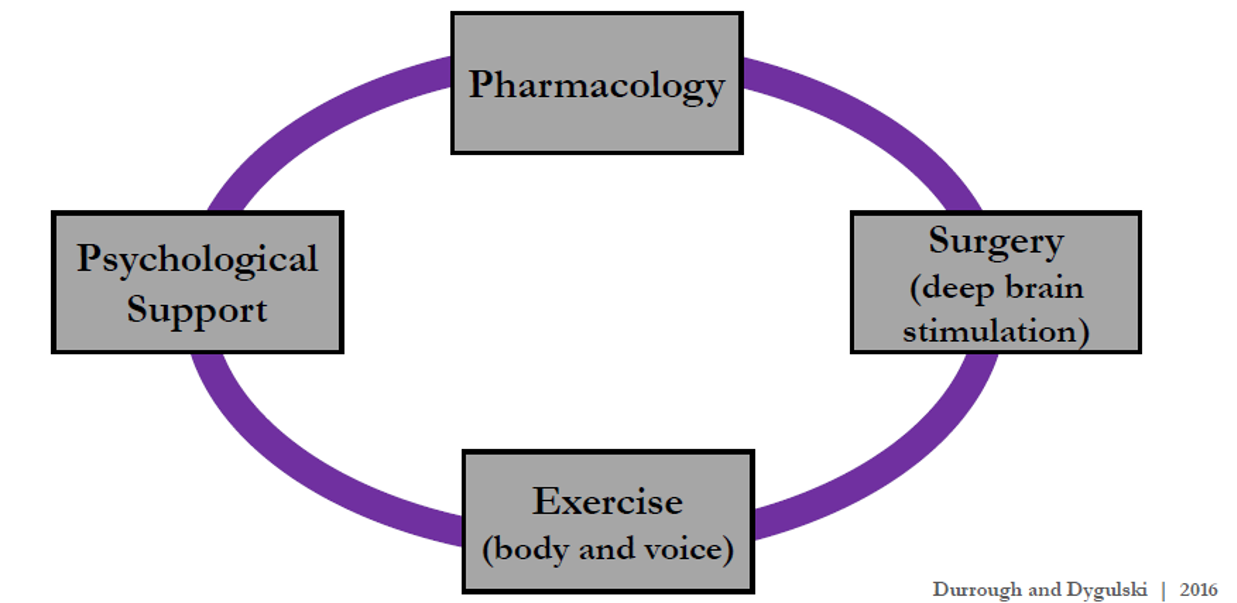
Pharmacological Management
Check out our blog post to learn about possible medical management.
Psychological Management
Check out our blog post to learn more about psychological support.
Exercise
Check out our blog post What is Parkinson’s and Exercise Prescription to learn more about how crucial exercise is to prevent and delay the progression of PD. In addition to the correct prescription for exercise!
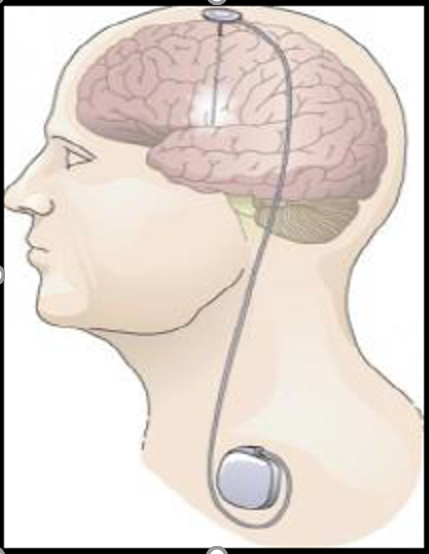
Surgery – Deep Brain Stimulation (DBS)
This surgery involves electrodes placed in the brain connected by wires to an implantable pulse generator under the skin of the chest.
Goal: to minimize “off” times, dyskinesia’s, and reduce medication dosages (lower side effects).
Limitations of DBS: Variable reduction in symptoms, postural stability not impacted, and risk for infection (as with any surgery).
Things to Remember!
Research continues to further our understanding of Parkinson’s Disease and more advanced treatment options. The important thing to remember is not everyone will have all the symptoms of PD and the type of symptoms and timing of progression varies. While there are numerous therapeutic options to manage Parkinson’s, EXERCISE is the ONLY DISEASE MODIFYING COMPONENT in the management of Parkinson’s Disease!
While we know exercise has great health benefits for all individuals, it is even more important for those with PD! Physical Therapy can also help address deficits and improve overall functional mobility and independence.
Goals of Physical Therapy
Slow progression
Optimize participation in home, work, and recreational activities
Optimize independence and safety with performance of functional tasks (gait, balance transfers, bed mobility, and ADL’s)
Preserve or improve physical capacity (strength, range of motion, endurance, etc.) .
Prevent falls
Exercise in Parkinson’s has been shown to:
Improve balance, gait, and activities of daily living
Increase stimulus-evoked release and decrease decay of dopamine in the dorsal striatum
Increase striatal dopamine
Delay and even prevent Parkinson’s disease in healthy individuals
Slow disease progression and motor deterioration
Increase corticomotor excitability
Improve UPDRS score – motor function and bimanual dexterity
Reduce rigidity and bradykinesia
Improve quality of life and reduce fatigue
Reduce falls
And the list goes on!
With all of the emerging research, the goal with exercise and proper medication management is to eliminate the end stages of PD. Speak with your Movement Disorder Specialist and reach out to us at NeuroLab360 with any questions you may have. Let’s fight Parkinson’s together and maximize your functional potential!
References:
LohleM, StorchA, Reichmann H. Beyond tremor and rigidity: non-motor features of Parkinson’s disease. J Neural Transm(Vienna). 2009;116(11):1483-1492.
VitekJL. Mechanisms of deep brain stimulation: excitation or inhibition. MovDisord. 2002;17:S69-72.
Parkinson's Disease Foundation. Primary Motor Symptoms. 2016. Available at: http://www.pdf.org/symptoms_primary. Accessed February 5, 2016.
Fisher BE, Wu AD, Salem GJ, et al. The effect of exercise training in improving motor performance and corticomotorexcitability in persons with early Parkinson’s disease. Arch Phys Med Rehabil. 2008;89(7):1221-1229.
PetzingerGM, Walsh JP, AkopianG, et al. Effects of treadmill exercise on dopaminergic transmission in the 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine-lesioned mouse model of basal ganglia injury. J Neurosci. 2007;27(20):5291-5300.
TillersonJL, Cohen AD, PhilhowerJ, Miller GW, ZigmondMJ, SchallertT. Forced limb-use effects on the behavioral and neurochemical effects of 6-hydroxydopamine. J Neurosci. 2001;21:4427-4435.